What is Diabetes?
Type 2 diabetes is a syndrome characterized by high blood sugar resulting from an impaired response to insulin. Type 2 diabetes is usually diagnosed in patients over the age of thirty, but it also occurs in children and teens. It is commonly associated with being overweight, especially around the abdomen area. Many times, it is diagnosed after a period of significant weight gain.
Symptoms of Diabetes
Type 2 diabetes is frequently diagnosed in aymptomatic patients during a routine medical examination. Symptoms of diabetes include:
- Frequent urination
- Thirst
- Weight loss
- Blurred vision
- Fatigue
- Nausea
- Fungal and bacterial infection
- Itching due to vaginal yeast infection
Late complications of diabetes include: heart disease, infections, skin ulcers, kidney disease, numbness and tingling in the hands and feet, impotence, constipation, pain and poor circulation in the legs, vision loss.
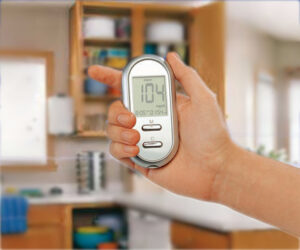
Diagnosis
Type 2 diabetes is diagnosed when the criteria for fasting high blood sugar are met. Blood sugar level is greater than or equal to 140 mg/dL (7.77 mmol/L) after an overnight fast on two occasions, or the American Diabetes Association criteria of fasting blood sugar greater than 126 mg/L (6.99 mmol/L) can considered to be diagnostic.
A test called the oral glucose tolerance test is often conducted if fasting blood sugar is between 115 and 140 mg/dL (6.38 and 7.77 mmol/L) and in those with a clinical condition that might be related to undiagnosed type 2 diabetes.
For monitoring diabetes, glycosylated hemoglobin (HbA1c) is tested to estimate blood sugar control over the prior three months.
Natural Treatments for Diabetes
Most people with this type of diabetes are treated with diet, exercise and oral prescription drugs. Some people require the use of insulin to control blood sugar. Several alternative methods may help when used under medical supervision in conjunction with standard treatments. Once herbs and other measures for controlling blood sugar work, medication needs to be adjusted by your doctor.
Diet
A balanced diet is recommended. Foods that emphasize vegetables, legumes, whole grains, and fiber can influence the release of sugar into the bloodstream. Foods that should be avoided are refined sugar, processed food, junk food, pastries, and cookies. When checking labels, watch out for hidden forms of sugar, such as dextrose, glucose, sucrose, corn sweeteners, fructose, dextrin, high-fructose corn syrup, lactose, modified cornstarch, maltose, malt, fruit juice concentrates, mannitol, sorghum, xylitol, and sorbitol. Protein snacks should be eaten in between meals. Alcohol, tobacco, and caffeine should be avoided.
All foods cause a varying insulin response in our bodies. Foods that have a higher rating on the “glycemic index”, a scale developed by nutrition researchers at the University of Toronto, cause a higher insulin spike than those with a lower rating.
Higher glycemic index foods are white bread, bagels, English muffins, packaged flaked cereal, instant hot cereals, frozen desserts, dried fruit, whole milk, hot dogs, and luncheon meat.
Lower glycemic index foods are most fresh vegetables, leafy greens, 100% whole grain bread, sweet potato, skim milk, buttermilk, chicken, lean cuts of beef, pork, and veal, white-fleshed fish, and many nuts. There are many factors that can influence glycemic index, such as cooking and preparation method.
Herbs, Nutritional Supplements and Vitamins
Chromium – Chromium is an essential trace mineral. It plays a major role in sugar metabolism. There is a growing body of evidence that shows that chromium may help bring blood sugar levels under control in type 2 diabetes. A typical dose of chromium for diabetes is 200 to 400 mcg per day.
Fenugreek – Fenugreek is a spice commonly used in India and the Middle East in cooking. Numerous studies suggest that fenugreek can reduce blood sugar and cholesterol levels in people with diabetes. Fenugreek seeds can have a bitter taste, so people sometimes prefer to take it in capsule form. A typical dose range is 5 to 30 g three times per day with meals. Known side effects of high doses include mild digestive distress. Fenugreek should not be used by pregnant or nursing women.
Gymnema – Gymnema is an Ayurvedic herb that is believed to have a marked effect on blood sugar control. Doctors often prescribe gymnema for mild cases of type 2 diabetes, in conjunction with standard treatments. A typical dose range is 400 to 600 mg per day of an extract standardized to contain 24% gymnemic acids.
Vanadium – Vanadium is an essential trace mineral that may mimic insulin to help regulate blood sugar. It is found in black pepper, dill seed, and unsaturated vegetable oil, as well as in vitamin supplements.
Zinc – Zinc is necessary for the normal production of insulin. Food sources of zinc include fresh oysters, ginger root, lamb, pecans, split peas, egg yolk, rye, beef liver, lima beans, almonds, walnuts, sardines, chicken, and buckwheat.
Other herbs and supplements – The function if the digestive organs should be optimized, particularly the liver and pancreas. Dandelion and other bitter herbs, tumeric, and bupleurum are just a few of the herbs that can help with this. Another goal should be to tonify the endocrine system and promote hormonal balance. Ginseng, licorice, oatstraw, and hawthorn are some of the herbs that can tonify the endocrine system.
Other herbs that can affect blood sugar are bitter melon, neem, and goat’s rue. Helpful supplements for diabetes are vanadium, B vitamins (especially vitamin B6), vitamins C and E, and coenzyme Q10.
Treating Complications of Diabetes
Lipoic acid – In Germany, the antioxidant lipoic acid is used widely for the prevention and treatment of peripheral neuropathy in diabetes. This complication usually develops after many years, and is a painful condition affecting the nerves. Lipoic acid occurs naturally in the body, and it is often reduced in people with diabetes. It is involved in the energy metabolism in the body. There is some evidence that lipoic acid may be more effective if it is combined with GLA (gamma-linolenic acid). A typical dose for diabetes is 300 to 600 mg per day, divided into two or three doses.
GLA (Gamma-Linolenic Acid) – An excellent source of the essential fatty acid is evening primrose oil. It is also found in black currant and borage oil. There is some research suggesting that evening primrose oil can protect nerves, and help with symptoms such as pain and numbness. A typical dosage is 4 to 6 g daily, taken with food. Evening primrose oil requires about six months to have noticeable effect. One caution, it is possible that GLA may worsen temporal lobe epilepsy.
Omega-6 oils should be taken in balance with omega-3 oils, found in flaxseed oil, pumpkin seeds, walnuts, and fish oil. Omega-3 fats can help protect blood vessels and decrease insulin resistance.
 For an individual with either type-1 or type-2 diabetes, the threat of hypoglycemia — commonly known as low blood glucose — is constant. Blood-sugar levels that drop too low present a variety of health risks, and exercise can cause blood-glucose levels to drop in both diabetics and those without diabetes. When exercising, it’s important to understand the relationship between physical activity, food intake and hypoglycemia.
For an individual with either type-1 or type-2 diabetes, the threat of hypoglycemia — commonly known as low blood glucose — is constant. Blood-sugar levels that drop too low present a variety of health risks, and exercise can cause blood-glucose levels to drop in both diabetics and those without diabetes. When exercising, it’s important to understand the relationship between physical activity, food intake and hypoglycemia.

 Insulin is a hormone. It makes our body’s cells absorb glucose from the blood. The glucose is stored in the liver and muscle as glycogen and stops the body from using fat as a source of energy.
Insulin is a hormone. It makes our body’s cells absorb glucose from the blood. The glucose is stored in the liver and muscle as glycogen and stops the body from using fat as a source of energy. Physician / Preventive Medicine Expert Explains How To Reverse Obesity And Diabetes Naturally
Physician / Preventive Medicine Expert Explains How To Reverse Obesity And Diabetes Naturally